Higher vitamin D levels seem to be linked to a reduced risk of early age-related macular degeneration. This chronic disease leads to degeneration of the macula, and is the main cause of irreversible vision loss in adults in developed countries. Approximately 8.5 million Americans aged 40 years and older are affected by age-related macular degeneration, or AMD. Data from 1,313 women was examined to see if serum 25(OH)D blood levels was linked to early AMD. Serum 25(OH)D being the preferred vitamin D status biomarker, as it reflects exposure to vitamin D from both sunlight and oral sources.[1]
No significant relationship was found between vitamin D status and early or advanced age-related macular degeneration after making adjustments for age and other known age-related macular degeneration risk factors. In women under 75 years, higher serum 25(OH)D levels was linked to a significantly reduced risk of early age-related macular degeneration, but in women 75 years and older, higher levels were linked to a significantly higher risk.
In women under 75 years, vitamin D intake from supplements and foods was linked to reduced risk of early age-related macular degeneration. Women with the highest vitamin D consumption had a 59% reduced risk of early age-related macular degeneration in comparison to women with the least vitamin D consumption. The main food sources of vitamin D were fish, milk, fortified cereal and fortified margarine. No relationship was seen making use of self-reported time spent in direct sunlight.
This is the 2nd study to show a link between 25(OH)D status and age-related macular degeneration, and supports the previous observation that vitamin D status could offer protection against development of age-related macular degeneration.
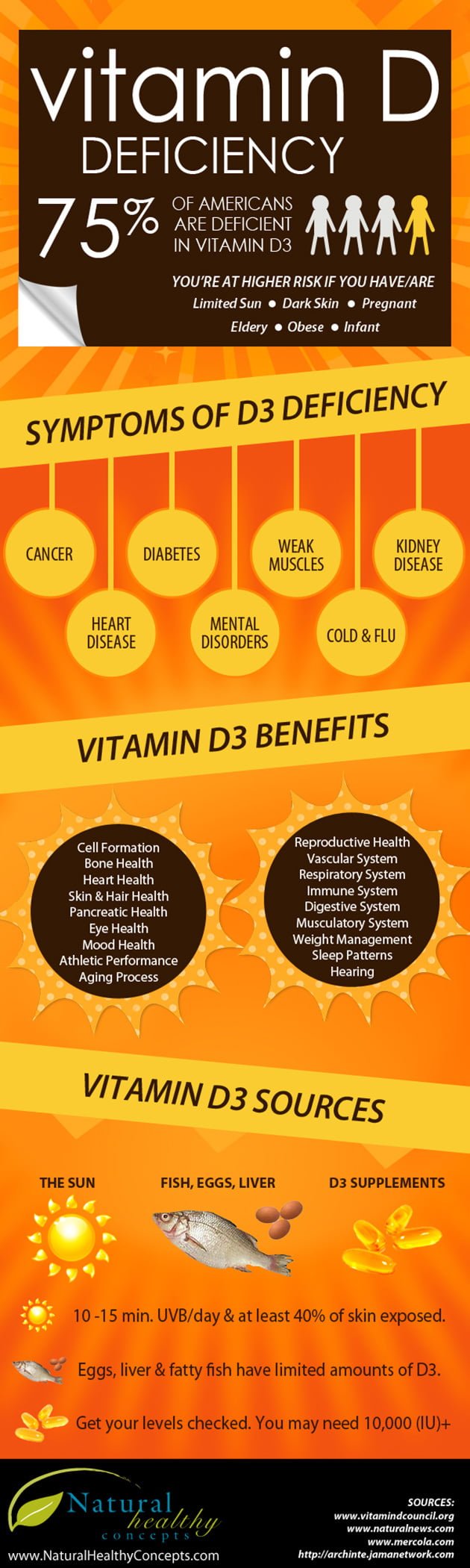
Image Source: Natural Healthy Concepts